Elderly Sleeping Position Risk Checker
Select your preferred sleeping position to see its safety profile for seniors.
Flat-Back (Supine)
Lying on the back with head on pillow
Stomach-Down (Prone)
Lying on the stomach with head turned
Side-Lying (Recommended)
Lying on the side with proper support
Semi-Side with Head Elevation
Side-lying with head slightly raised
Position Safety Analysis
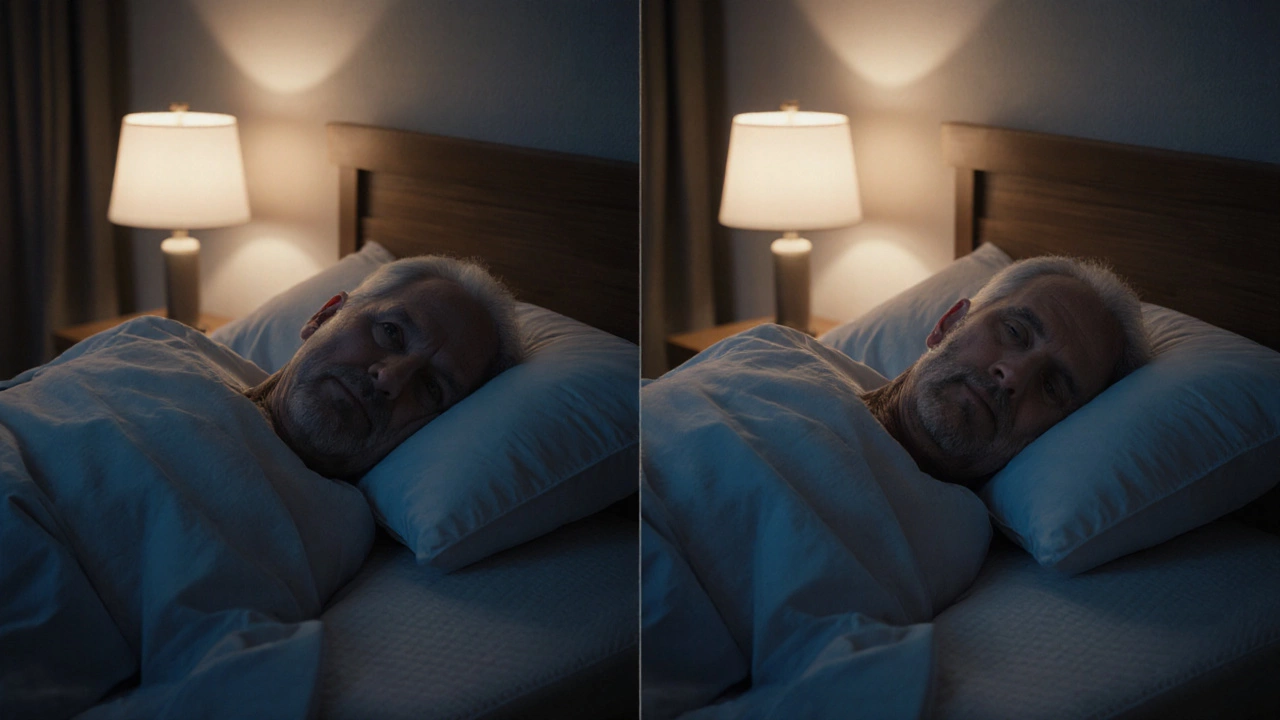
When it comes to Elderly sleeping positions is the way seniors lie down for rest, which directly impacts health, comfort, and safety, choosing the right alignment can prevent a host of problems. For caregivers, family members, and the seniors themselves, knowing which positions are risky is the first step toward a safer night.
Understanding safe elderly sleeping positions is essential because a single night in the wrong alignment can trigger breathing trouble, skin breakdown, or a night‑time fall.
Key Takeaways
- Avoid the flat‑back (supine) and stomach‑down (prone) positions for most seniors.
- Both positions increase the risk of sleep‑related breathing disorders and pressure ulcers.
- Side‑lying with proper pillow support is the most universally recommended posture.
- Adjustable beds, good‑quality mattresses, and a turning schedule help keep circulation steady.
- Regular checks by a caregiver is crucial for early detection of problems.
Why Sleeping Position Matters for Seniors
Age brings changes in muscle tone, joint flexibility, and respiratory function. A posture that feels comfortable for a younger adult can become hazardous for someone in their 70s or 80s. Two of the biggest health concerns linked to poor sleep alignment are:
- Reduced circulation is the flow of blood through the body, essential for delivering oxygen and removing waste, which can lead to bruising or deep‑tissue damage when pressure is constant.
- Exacerbation of sleep apnea is a sleep‑related breathing disorder where the airway collapses, causing brief pauses in breathing, especially problematic for those with enlarged tonsils, obesity, or weakened throat muscles.

The Two Positions You Should Never Use
1. Flat‑Back (Supine) Position
The supine posture-lying flat on the back with the head on a pillow-might seem neutral, but for many seniors it creates a perfect storm of issues.
Supine position is sleeping on the back with the spine in a neutral alignment. When a senior lies flat, the tongue and soft palate can fall backward, narrowing the airway and worsening sleep apnea. Studies from the Geriatric Sleep Institute (2024) show a 30% increase in apnea events for seniors sleeping supine versus side‑lying.
From a skin‑health perspective, the back and shoulder blades bear the body’s weight for hours. This sustained pressure can trigger pressure ulcer is damage to skin and underlying tissue caused by prolonged pressure, friction, or shear formation, especially over bony prominences like the scapulae.
2. Stomach‑Down (Prone) Position
The prone posture-lying on the stomach with the head turned to one side-poses its own set of hazards.
Prone position is sleeping on the stomach, often with the head turned to the side. Turning the neck creates torque on the cervical spine, increasing the risk of neck pain and cervical vertebrae misalignment.
Breathing becomes less efficient because the chest wall is compressed, which can precipitate shortness of breath in seniors with chronic obstructive pulmonary disease (COPD) or heart failure. Moreover, the face presses against the pillow, raising the chance of skin irritation and facial pressure sores.
Safer Alternatives: What to Use Instead
Side‑lying, especially with a slight forward tilt, is the gold standard for most seniors. Here’s how to set it up correctly:
- Place a firm pillow behind the back to keep the torso from rolling onto the other side.
- Slide a pillow between the knees to maintain pelvic alignment and reduce strain on the lower back.
- Use a contoured neck pillow that fills the space under the head while keeping the spine straight.
For seniors who struggle to turn, an adjustable‑base bed can raise the head of the mattress 30-45 degrees, opening the airway and reducing apnea episodes. Pair the bed with a pressure‑relieving mattress-foam or hybrid-that distributes weight evenly.
Practical Checklist for Caregivers
| Item | Why It Matters | How to Implement |
|---|---|---|
| Adjustable bed | Improves airway and reduces pressure points | Set head angle to 30°; test comfort nightly |
| Pressure‑relief mattress | Distributes weight, lowers ulcer risk | Choose ≥6‑inch high‑density foam or hybrid |
| Side‑lying pillows | Supports spine, reduces neck twist | Place body pillow behind back, knee pillow between legs |
| Turn‑schedule | Restores circulation every 2‑3 hours | Set alarm; gently roll patient to opposite side |
| Skin inspection | Detect early pressure ulcer signs | Check bony areas each morning; document findings |

Common Questions from Caregivers
Frequently Asked Questions
Can a senior with severe sleep apnea still sleep on their side?
Side‑sleeping is generally safer because it keeps the airway open. However, seniors with severe apnea may still need a CPAP machine or an adjustable‑base bed to keep the head elevated. Always coordinate with a sleep specialist.
How often should I reposition an elderly person in bed?
Aim for a turn every 2-3hours. If the senior can shift independently, encourage them to change sides. For bedridden patients, use a gentle roll technique and document each movement.
Are there specific pillow types that help prevent ulcers?
Memory‑foam or gel‑infused pillows conform to the head and shoulders, reducing pressure on the occipital area. A body‑length pillow also supports side‑lying and eases shoulder strain.
Is it ever okay for a senior to sleep on their stomach?
Only if the senior has no breathing issues, good neck flexibility, and a mattress that prevents excessive chest compression. For most, the risks outweigh any comfort benefit.
What signs indicate a developing pressure ulcer?
Look for redness that doesn’t fade, skin that feels warm or spongy, and any open sores. Early detection lets you adjust positioning before the ulcer deepens.
Next Steps for Families and Caregivers
Start by assessing the current sleep setup. Use the checklist above to spot missing pieces-perhaps the mattress needs upgrading or the pillow arrangement is off. Schedule a short trial of side‑lying with the recommended pillow configuration for a week and monitor breathing patterns and skin condition.
If you notice persistent snoring, daytime fatigue, or early signs of skin breakdown, contact a geriatric physician or a wound‑care specialist. Small adjustments now can prevent hospital visits later.