When you sink into a recliner chairs after a long day, the comfort feels instant. But if you’ve been diagnosed with degenerative disc disease (DDD), that cozy moment can raise a red flag. Below we break down how recliners interact with a fragile spine, what to watch for, and how to enjoy relaxation without worsening the condition.
Understanding Degenerative Disc Disease
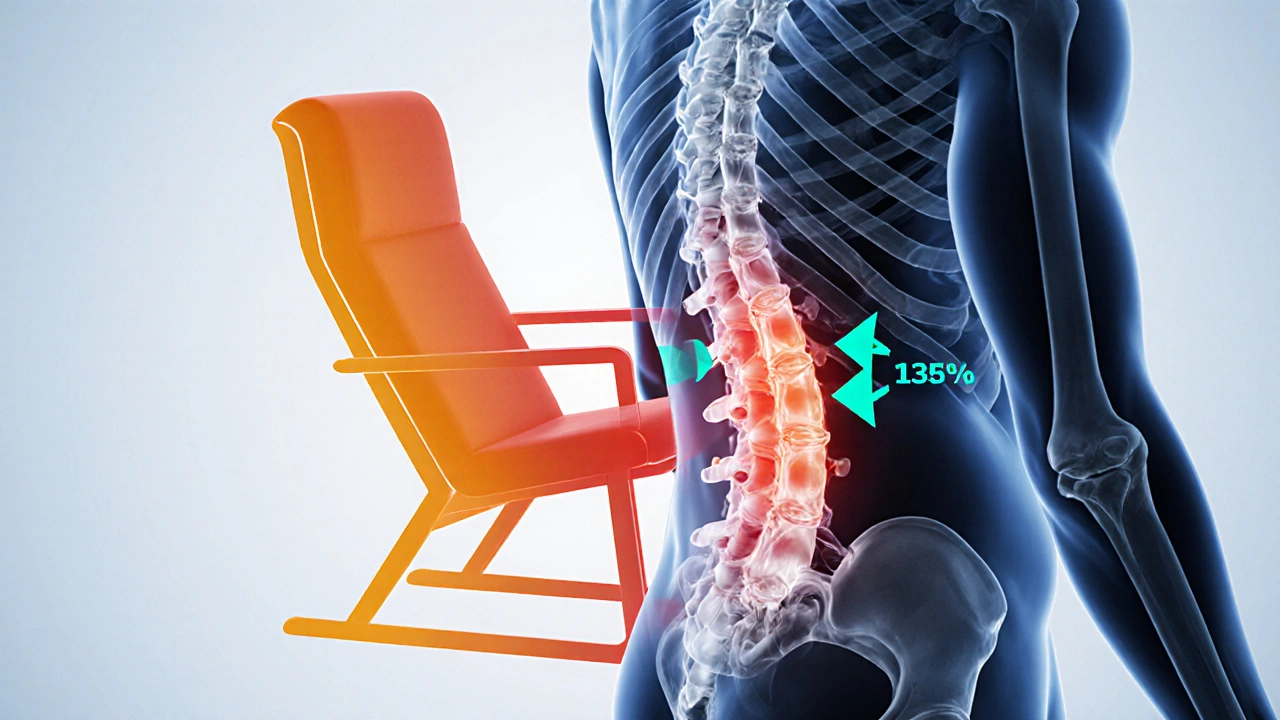
Degenerative Disc Disease is a condition where the intervertebral discs lose hydration and elasticity, leading to reduced shock absorption and potential pain. It’s not an actual disease but a description of disc wear and tear that happens with age, injury, or genetics. The key players are the intervertebral disc, a gel-like core (nucleus pulposus) surrounded by fibrous cartilage (annulus fibrosus). As these discs thin, the vertebrae sit closer together, altering spinal alignment and sometimes causing nerve irritation.
Typical symptoms include chronic low‑back ache, stiffness, occasional leg tingling, and reduced flexibility. Diagnosis often involves magnetic resonance imaging (MRI), which visualizes disc hydration levels and any herniation.
What Makes a Recliner Different?
Recliner Chair is a type of upholstered seat that tilts backward, often with a footrest that lifts the legs. Its design aims to distribute weight across the back, seat, and legs, reducing pressure on any single point. Modern recliners boast lumbar support, adjustable headrests, and sometimes memory‑foam cushioning that conforms to the body.
Contrast that with a standard armchair, which stays upright and generally offers a fixed back angle. The reclining motion can be beneficial for circulation, but it also changes the curvature of the lumbar spine-a critical factor for DDD sufferers.
How Reclining Affects a Degenerative Spine
When you tilt a recliner back, the lumbar curve typically flattens, moving the spine toward a more neutral or even kyphotic position. For a healthy disc, this shift relieves compression. However, in DDD the disc already lacks cushioning, so a flattened curve can increase shear forces on the annulus fibrosus, potentially accelerating wear.
Research from the Journal of Orthopaedic Research (2023) found that prolonged reclining beyond 30 minutes raised intradiscal pressure by up to 12% compared with an upright sitting posture, especially when the recline angle exceeded 110°. The magnitude varied with the chair’s ergonomic design-chairs with built‑in lumbar support mitigated the pressure rise by about half.
Key risk factors include:
- Extended recline sessions (over 45 minutes) without changing position.
- Recliners lacking adjustable lumbar pads.
- Improper footrest height that forces the knees into a tight angle.
- Existing severe disc collapse (grade III or higher).
Safe Reclining Practices for DDD
If you love the feeling of a recliner, you don’t have to ditch it completely. Follow these evidence‑backed steps to keep pressure on the discs at a minimum:
- Set a moderate angle. Aim for a 100‑110° recline (roughly a 30‑40° tilt). This keeps the lumbar curve gentle rather than flat.
- Engage lumbar support. If your chair has an adjustable pad, raise it until you feel a small “dip” in the lower back that supports the natural curve.
- Adjust the footrest. Your knees should form about a 90° angle when the footrest is up. Too high creates strain on the lower back and hamstrings.
- Limit time. Use a timer-no more than 30 minutes continuous. Stand, stretch, or walk for a minute or two before a new recline.
- Incorporate cushions. A thin, high‑density lumbar pillow can replace built‑in support if the chair lacks it.
- Stay active. Pair reclining with core‑strengthening exercises (e.g., bird‑dog, plank variations) at least three times a week to improve spinal stability.
These adjustments mimic the best practices recommended by physical therapists at the American Physical Therapy Association (APTA) for patients with chronic back conditions.
Alternative Seating Options
When the recliner still feels risky, consider these alternatives that maintain comfort while encouraging better posture:
| Feature | Recliner Chair | Standard Armchair | Ergonomic Task Chair |
|---|---|---|---|
| Adjustable lumbar support | Yes (if model includes) | No | Yes - customizable |
| Recline angle range | 70°‑130° | Fixed upright | 0°‑20° tilt |
| Weight distribution | Back, seat, footrest | Back & seat only | Dynamic seat pan |
| Ideal for prolonged use | Medium - needs breaks | Poor - static posture | High - promotes micro‑movement |
| Cost (average US$) | 400‑900 | 150‑300 | 250‑500 |
Notice that an ergonomic task chair scores higher for continuous daily use because it encourages subtle shifts in posture, keeping disc pressure more evenly distributed.

When Reclining Is a Red Flag
Even with precautions, some signs mean you should stop using the recliner and see a specialist:
- Sharp, shooting pain that radiates down the leg after a recline session.
- New numbness or tingling in the foot or toes.
- Persistent stiffness that worsens the next day.
- Loss of balance when getting up from the reclined position.
If any of these appear, schedule an appointment with an orthopaedic spine doctor or a qualified physical therapist. Early imaging (MRI) can reveal whether the disc has further degenerated or if a herniation has occurred.
Quick Checklist for Safe Reclining
- Recline angle: 100‑110°.
- Lumbar support: engaged and snug.
- Footrest: knees ≈ 90°.
- Time limit: ≤30 min per session.
- Break routine: stand/stretch every 20 min.
- Core work: 3 × week.
- Watch for warning symptoms.
Frequently Asked Questions
Can a recliner cure back pain caused by DDD?
No. A recliner can ease momentary discomfort, but it does not reverse disc degeneration. Long‑term relief comes from targeted exercise, posture correction, and medical management.
Is there a safe recline angle for anyone with a weak lower back?
For most people with mild DDD, staying between 100° and 110° minimizes shear on the lumbar discs while still offering a relaxed position.
Should I buy a recliner with built‑in heating or massage?
Heat can temporarily soothe muscle spasms, but massage paddles that press hard on the spine may aggravate a fragile disc. Choose low‑intensity heat only, and avoid deep‑tissue massage functions.
How often should I replace a recliner if I have DDD?
If the cushioning compresses or the lumbar support loses shape, it’s time to replace it-usually every 5‑7 years for quality models. Worn padding can increase pressure on the spine.
Are there specific exercises to do before using a recliner?
Gentle cat‑cow stretches and a 30‑second plank help activate the core and promote spinal alignment, making the subsequent recline feel safer.
Enjoying a recliner isn’t off‑limits for everyone with degenerative disc disease, but it does require a smarter approach. By respecting angles, supporting the lumbar curve, limiting time, and staying active, you can relax without throwing your back into overdrive.



